cath lab display screens free sample
Setting up a cath lab with all the right options for your specialty, your workflow, and your physicians" preferences comes with a lot of questions. Among those we"re asked most often: How many monitors come with a cath lab system?
The answer to that question isn"t 100% cut-and-dry, but we can help you know what to expect as you begin shopping. Keep reading to learn more about monitor options for your next cath lab system.
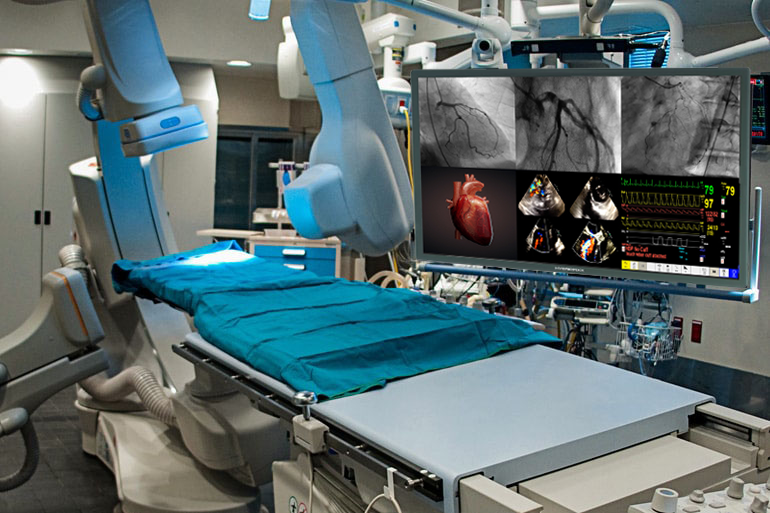
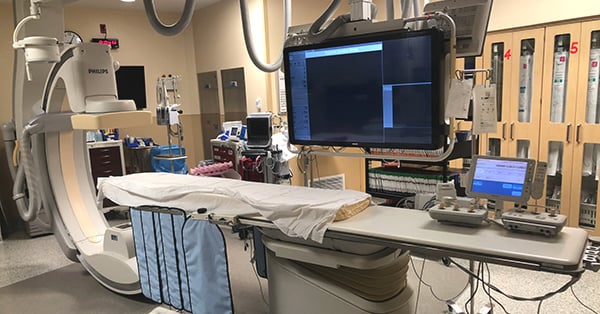
Typically, cath labs come with just 2 monitors included on the monitor suspension arm: a live monitor, and a reference monitor. Seems like an easy enough answer, right?
The extra positions on the monitor suspension are for, you guessed it, extra monitors! Okay, that’s a bit of an over-simplification, so let us explain. In the cath lab, more than any other modality, peripheral systems are used to help treat the patient. Depending on what these systems are and how many you have, it may be preferable to add one, two, or even six more monitors onto your suspension.
Most cath labs use a hemodynamic monitoring system such as a GE MacLabduring studies. There is often a monitor on the suspension that displays the patient"s physio data in real time so the staff has immediate feedback from the MacLab.
If you’re in a lab that performs 3D studies, there is a good chance the cath lab itself is unable to reconstruct the raw data acquired during a study. In this case, a reconstruction workstation such as a GE Advantage Windows Workstation (AWW) is needed to reconstruct the images. When a reconstruction workstation is in use, one of the monitor slots on the suspension can be dedicated to displaying reconstructed image data.
When a site orders a new cath lab from the manufacturer the number of spaces available on the monitor suspension can be selected. If you plan to purchase your lab on the secondary market, be sure to talk to your provider early on about how many monitor spaces you"ll need so they can accommodate. For single-plane labs, suspension systems are available with two to six monitor spaces. Suspensions for up to eight monitors are available for biplane systems.
If you have additional questions about monitors or monitor suspensions, are in need of a cath lab, or need some peripheral equipment to help fill out your monitor suspension, call or email us today

Strangely enough, the argument went, many of the same skills to be good at Mario Kart or Call of Duty were important in manipulating laproscopic surgical instruments. In an odd way, what is being said is that visual-spatial thinking, hand-eye coordination, and other similar skills are becoming increasingly critical with minimally invasive interventions that require the operator to convert 2D images on a screen into 3D anatomy – a skill that means the difference between removing a gall bladder properly verse perforating the bowel. Virtual Cath Lab is a free app that is great example of how medical educational can use new training modalities to prepare trainees for this shift.
When performing a cardiac catheterization, the interventionalist must mentally translate a two-dimensional, black-and-white image into a three dimensional heart. Complicated by the fact that there are really no landmarks on the screen to help orient the viewer, it takes a lot of practice and time to learn the different projections and translate them into a usable mental model. But with apps like this, that time can be shortened.
The app itself has a very simple interface – basically a C-arm with a “patient” and an inset window with the screen that would be displayed. The user can rotate the c-arm using the touchscreen and will see in the inset window the view of the heart change. Tapping the menu button cycles through several different option menus. The two key ones are the Sequencer and the Fluoro Suite Controls.
The sequencer is basically a menu of several standard cath lab views. For someone trying to orient themselves to the black-and-white screen images displayed in the cath lab, this app is quite useful in terms correlating say an RAO caudal projection on the screen to the cardiac anatomy.
The second main menu involves various cath lab controls, such as the ability to move the table, move the patient, change your viewpoint of the table, and so on. Basically, it gives you a few more options in terms of optimizing the set up to mirror more closely your own learning environment.
There are however several points of improvement for this app. The actual coronary vasculature is not displayed on the heart, making correlating the cath lab images to the anatomy a bit more challenging. Also, inclusion of some actual cardiac catheterization images would be helpful in allowing one to practice and learn correlating the images to real anatomy.
All in all, the app is a great example of how the iPhone, iPad, and other similar consumer devices combined with some ingenious developers can really enhance medical education. Virtual Cath Lab is definitely a step up from trying to learn how to use these images from an anatomy textbook, heart model, or other more traditional educational methods.

A catheterization laboratory, commonly referred to as cath lab, is a vital piece of diagnostic equipment for hospitals and healthcare facilities. A cath lab is an exam room equipped with diagnostic imaging technology to provide physicians with visual access to chambers and arteries of the heart. In these spaces, a team of physicians perform life-saving procedures, including coronary angiography, catheterization, balloon angioplasty, percutaneous coronary intervention, congenital heart defect closure, stenotic heart valves and pacemaker implantations. A typical cath lab consists of a C-arm, image intensifier, X-ray tubes, and several displays.
Cath lab operations depend completely upon medical displays, which allow physicians to visualize a patient internally and perform the necessary procedure. The digital age has ushered in improved imaging technologies, which emit less radiation and also provide greater visual clarity to physicians. The adoption of CRT monitors in the cath lab brought about significant changes in their operations. CRT displays were followed by the advent of LCD screens. Most hospitals and healthcare facilities upgraded to LCD screens as they are slimmer, portable and offer higher resolution images. Currently, cath labs are witnessing yet another transition in medical monitors, as professionals are upgrading from LED displays to ultra-high definition 4K technology. Instead of using four to six displays, hospitals and healthcare facilities are upgrading to one large UHD 4K display. However, healthcare providers need to consider several variables before deciding upon the kind of upgrades they can make. Additionally, the switch from the LED model to the 4K display system introduces issues related to maintenance and safety.
Ampronix (Irvine, CA, USA), an authorized master distributor of the medical industry"s top brands and a manufacturer of innovative technology, has been repairing and selling 4K monitors of different sizes for cath labs and hybrid ORs to hospitals for years. Ampronix undertakes sale, service and repair of cath lab monitors manufactured by several well-known companies such as Philips, GE, Siemens, Shimadzu, Toshiba, Hitachi, Eizo, Barco, Chilin and Optik View. Ampronix offers tailored, one-stop solutions at a faster and more cost effective rate than other manufacturers. The company has most models in stock that are available at half the OEM price.
The company’s services also include preventive maintenance, replacement of LCD, backlights, reflectors and power supplies. Any display failure amounts to an entire cath lab rendered obsolete until a replacement or repair solution is provided. However, the turnaround time for either of those protocols can be several weeks. Given the importance of the cath lab for healthcare providers, Ampronix ensures that they have zero downtime in the event of their monitors requiring service or replacement. The company has a readily available response team of ESD- and ASQ-certified technicians to assist and answer questions for urgent repairs. Nation-wide requests received by 2pm PST receive same-day or next-day delivery. Ampronix also has capable and competent customer service representatives for addressing all medical technology questions and concerns. With its extensive product knowledge, outstanding service, and state-of-the-art repair facility, Ampronix continues to meet the needs of the medical community and move forward with its goal to facilitate optimized patient care and improved physician workflow.
In the rural setting where I practice, there is only one hospital in the entire county. There is no other hospital within an hour’s drive to take my patients to and perform catheterizations that wouldn’t disrupt the patient flow in my clinic. I knew there had to be a better way. I put my thoughts on paper in terms of requirements and wishes, and decided to learn what was required by my state to open and operate an outpatient cardiac cath lab. I knew that designing the space to permit smooth patient flow would be the easy part — anyone who has spent their career working in a cath lab has ideas of “if I was building a new cath lab from scratch, I would make sure I included A, B, and C”.
Two prior cardiac cath labs had existed in Alabama in years past, but were shuttered due to newly enacted laws that limited their scope. Once I determined that those state laws had since been modified, I knew the time was right. I spent a great deal of time conducting my own feasibility study — determining what payor would reimburse for outpatient procedures, reviewing my own volume, and creating a proforma, as well as researching what certification or credentialing would be required. I decided to use existing, unbuilt space in the main level of my two-story office to construct a cardiac cath lab, applying all the lessons I have learned about cath lab workflow over my career.
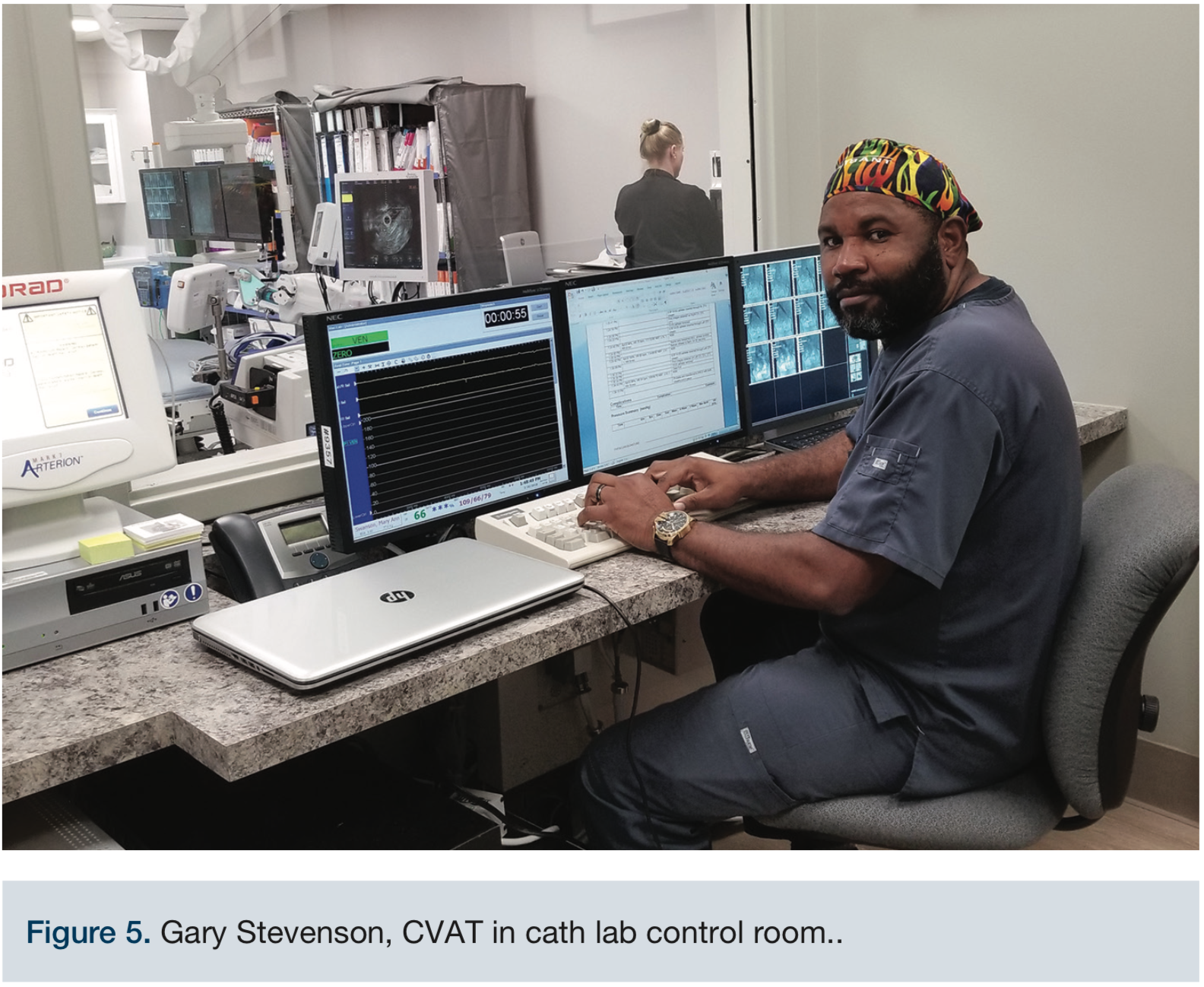
Cardiac catheterization requires hemodynamic parameter monitoring functionality that is not necessarily required by a vascular lab. The critical component is the hemodynamic monitoring software and hardware. Several versions exist — Mac-Lab (GE Healthcare), Witt (Philips), McKesson, and other proprietary softwares. This software provides rhythm strips, hemodynamic monitoring, and the ability to scribe the sequence of events in the classic “control room” that all cardiac cath labs have. Vascular labs do not typically require hemodynamic monitoring outside of a rolling sphygmomanometer, and maybe oximetry. End tidal CO2monitoring may be added if significant sedation is required. In some states, including the state in which I work, the law states that the citizens of that state cannot undergo cardiac angiography in a non-fixed cath lab setting (mobile C-arm). Therefore, a floor-mounted or ceiling-mounted x-ray suite is required to perform heart catheterizations in some states.
The first step is determining the need. The need of the community, the need of your patients, and the need of the practice itself. Once a need has been established, then estimate the number of potential cases that can be appropriately performed in an OBL setting. At this point, don’t factor in the growth that will happen from marketing and word-of-mouth. If you determine that sufficient volume exists to justify a deeper look, then involve your healthcare attorney and your billing company. By creating a proforma of all the types of procedures you intend to perform in an OBL, you can determine if your venture will float, and if so, the specific volume you need to break even. Meet with an architect familiar with healthcare applications to determine a ballpark estimate for cost of construction, and add 30% to that estimate. Discuss with your banker the financing arrangements available to you, including your own cash infusion and working capital on the tail end. To determine how much working capital you will require, have a discussion with several interventional product suppliers about net 30/60/90 payment options. As you can imagine, there are many moving parts, and you need each piece of information to help determine other pieces of information. If this makes you dizzy, you may want to hire a consultant who builds OBLs for a living. If this proposition excites you, then read on!
Due to the considerable time and cost investment to open an OBL, due diligence is required before expending the resources. Assessment of your current case mix is first — do you have more cases than you can get on the schedule at the hospital where you work? Do you have a considerable backlog of peripheral interventions waiting for a time slot? Are there untapped geographical regions to which you can market, and that would allow you to grow your existing referral base and volume? Would your local hospital attempt to interfere with your plans, or outright oppose it with the state in which you practice? Would your local hospital try to retaliate against you for steering patients away from their facility? Do you have the resources available to fund construction? What cases do you wish to perform in an outpatient setting? Are you willing to seek further training to perform different types of cases (fibroid embolization, dialysis graft access work, etc.) from the bread-and-butter peripheral intervention? Would your vendors assist you in consignment inventory and training opportunities? Do you have access to trained cath lab staff or would they need on-the-job training? How many staff members would you want present in a given case at a given time? Who would handle your billing? Would you hire a professional coder, or would you have your physicians attending coding classes and be responsible for coding properly? Would you participate in registries? Would you seek accreditation? Who would handle staffing, staff education, and staff certification of competencies?
I was fortunate to find a very helpful individual within the State Health and Planning Development Agency (SHPDA) who provided me with the “denial letter” from a previous applicant that spelled out the agency’s requirements. In my letter, I made sure that my proposed lab satisfied all their requirements. My proposal was posted on a public discussion board for 8 weeks, during a “public comment period”. This period is intended to allow ample time for any entity to object to an application for a Certificate of Need (CON). However, my request was not for a CON, but for a letter of non-reviewability. I was requesting acknowledgement that my facility was exempt from their oversight — that rationale was rooted in another state law that provides for the ability of a physician to build and open an operative suite within the walls of their primary medical office. My request was uncontestable by the only hospital within the service area of my office, codified by state law. After the obligatory public discussion period, I received a letter from SHPDA with their conditions to proceed.
If we had elected to construct in a freestanding building, the local hospital could have offered resistance and tried to delay our progress by contesting our need to build a cath lab. Since we built inside the four walls of our existing medical office, we were protected by statute written into the code of the state of Alabama. No one could contest our right to build a cath lab within our own office.
This depends on your organizational skills. If you are a detail-oriented planner who can create timelines and flowcharts of all the tasks required to open an OBL, then you do not need to partner with a company that builds cath labs for a living. Typically, these companies go 50/50 with you on investment, and they build hospital-style cath labs, meaning that the cost of a lab they design would be roughly double what you could do by yourself. In return, they take 50% of the gross revenues in perpetuity. Forever. This percentage may be higher if they are managing the lab once it opens.
In my experience, I navigated the state regulatory agencies with relative ease and located a builder capable of constructing the space. The biggest challenge we encountered was an electrical engineer with the architect who insisted on planning our office-based lab with the backup and redundancy of a hospital facility. Since OBLs don’t deal with critically ill patients, patients on a ventilator, or trauma patients, the electrical requirements are different. OBLs do not require a fire alarm enunciator system. Since very few OBLs have been built in our region, the electrical engineer’s only experience was with hospital labs and he refused to acknowledge that an OBL did not need those costly features. Fortunately, our electrician was exceptionally talented. He followed the detailed construction plans provided by one of our established vendors and complied with local building code, creating a facility that operates efficiently and safely. Construction took us approximately 9 months, and we finished on budget.
Constructing a fixed ceiling-mount or floor-mount cath lab requires lead shielding of the interior walls, which are not required with a mobile C-arm. Shielding doors, windows, and walls becomes expensive, depending on what is on the other side of those walls. Exterior walls do not need to be shielded.
We opted for the latest A/V technology and thus have the capability of video conferencing between the cath lab itself and any other location with web camera capabilities. We constructed a conference room with three 4K monitors connected to micro-PCs, recessed screen with HD projector, and video conferencing. Surprisingly, this did not add much to the cost of the product, but added considerable functionality.
There is no patient access between the lower level cath level and the second level medical office. Installing a commercial elevator would add approximately $100,000 to the cost of the construction, and countless delays with engineering work, not to mention additional upstairs construction work to create an elevator shaft. Our building is on a grade. The upper level has a parking lot at that level, with handicap accessible ramp, and the entire main level is “barrier free” to comply with the Americans with Disabilities Act (ADA). We instruct patients coming for a procedure to park on the lower side of the building and enter through that entrance, which in the future will make a convenient arrangement to operate an ambulatory surgery center (ASC), complete with its own access.
We designed a dual-sided control room sandwiched by two 20 ft x 28 ft procedure suites. One of the procedure suites became our functional cath lab, and the other was left open for future growth. We currently use that room to host large groups, such as when we held an open house event or hosted a group of 30 business leaders in the community. Eventually, it may be built out as a computed tomography (CT) scanner suite or another angio suite. There is a physician office attached to the control room. The cath lab’s main door opens to a 5-bed PACU with a nursing station. On the other side of the PACU are two vein ablation rooms. The goal was to be able to flip-flop between rooms such that one patient could be getting greater saphenous vein (GSV) mapping while the other room was being used for the ablation procedure. By the time the endovenous laser therapy (EVLT) was complete, the next patient was ready to begin. We have a clean utility room, a dirty utility room with autoclave, two staff offices, an exam room, several storage rooms, and the high-tech conference room. The waiting room seats 16 and there is a small reception office. All the restrooms have five photocell sensors — light switch, flush valve, soap dispenser, faucet, and paper towel dispenser. The light switch is on a 10-minute timer. Most of our electrical outlets include USB plugs to charge wireless devices. Each bay in the cath lab has its own ceiling-mounted television.
From start to finish, construction took 9 months. This was an interior buildout with minimal exterior work — one overhead door had to be removed, framed and bricked in, another exterior door had to be cut. Front doors were replaced. Other than that, all the work was interior buildout, so weather had minimal impact on the timeline. The company that refurbished and certified our Siemens cath lab unit kept in close contact with our contractor so that there was no delay from when the room was ready to accept the x-ray equipment to complete installation of the cath lab room itself, the mechanical room, and the control room.
Having worked in cath labs for 18 years before opening our own, we had seen lean operations, well-staffed labs, and everything in between. To balance safety and efficiency, we decided on a staff of five: a monitor tech, a scrubbed assist, a circulating RN, a PACU RN, and a PACU medical assistant, plus the physician. If we are having a particularly busy day, we will pull another medical assistant from upstairs. Since we recover our own patients, it was important to have sufficient staff so that the workflow can proceed smoothly, regardless of the number of cases that day. As the physician of record, I try not to leave my staff alone with a patient unless I absolutely have to be somewhere else. They appreciate the camaraderie, and the physician’s willingness to help, even though they don’t need my help!
We have multiple biphasic Zoll defibrillators with a fully stocked hospital crash cart in the cath lab itself, a duplicate setup in the PACU, and a third identical setup in our nuclear medicine lab. We keep Wallgraft stents (Boston Scientific) on the shelf in the event of a peripheral arterial dissection with vascular compromise, coronary guides, coronary balloons and coronary stents in the event of a coronary dissection with hemodynamic compromise, and we have an intra-aortic balloon pump (IABP). We perform competencies on the IABP on regular intervals. All our staff is advanced cardiac life support (ACLS) certified. The crash cart contains intubation supplies, and we have suction and oxygen in the procedure room.
We met with all the product vendors, explained our plans, and requested that they develop a consignment inventory suitable to our needs. We work with Boston Scientific, Ra Medical Systems, Abbott, Biotronik, Cordis, and several others. The higher cost products such as stents, balloons, intravascular ultrasound catheters, wires, guides, and sheaths are consigned. We periodically review our consignment inventory, review par levels, and adjust our inventory on hand with our projected product usage. Products typically arrive two to three days after we order them, so we do not need to keep more than a month’s inventory on hand. We do keep IABP catheters, covered stents, and emergency products on hand that we hope will expire on the shelf. These products are typically not consigned, but we happily replace expired emergency products as the cost of doing business. We constantly price-compare between vendors for disposable supplies — we use Medline, Merit, McKesson, and US Endovascular, as well as several smaller vendors for specialty items like RadPads (Worldwide Innovations & Technologies).
Currently, there are two American College of Cardiology (ACC) outpatient registries: the PINNACLE registry and the Diabetes Collaborative Registry. We are planning to participate in the PINNACLE registry. While this database readily communicates with our current electronic health record (EHR), Amazing Charts, we are in the process of determining if it will communicate seamlessly with MedStreaming, the EHR to which we will be transitioning in the next six months.
As patients come to experience the convenience of OBLs, and as payors discover the cost savings of OBL procedures, there will be a deliberate paradigm shift to the outpatient setting, free of a hospital. In this environment where scrutiny is increasing on the cost of procedures, the OBL shines as a way to reduce expense and still deliver high-quality care. Patient satisfaction increases, complications decrease (fewer handoffs between departments, fewer access site complications with radial artery access), and patient co-payments decrease. I foresee a trend to perform as much in the outpatient setting as possible. Injectable loop recorders are expected to get an outpatient procedure code in 2020. We will petition the local state quality agency (in our case, the Alabama Quality Assurance Foundation) to embark on a pilot program to expand our offerings, such as pacemakers. Despite all the posturing and rhetoric from both sides of Congress, I do not expect any dramatic changes in the next 12 months.

Cardiac catheterization (also called a cath) is a minimally invasive procedure. During the procedure, a tiny catheter is guided into the heart, usually through a blood vessel in the leg or arm. Once inside the heart, it can be used to diagnose a problem or to treat a problem.
By gaining access to the beating heart, cardiac catheters allow a physician to check the internal blood pressure of the heart, assess blood supply, view the coronary arteries on the surface of the heart and check the level of oxygen in the blood. It is also used to evaluate the pumping chambers and to assess valvular function.
Cardiac catheterization is one of the most accurate tests in the diagnosis of coronary artery disease, and over a million of them are performed each year.
During cardiac catheterization, the physician tracks the course of the catheter by watching it on a fluoroscope, an x-ray machine that displays the catheter and blood vessels in real time on a screen. A variety of measurements may be performed when the catheter is in place. Once the catheter is removed, patients are given 6 hours of recovery time, and most patients are free to go home. Results are often available within a matter of hours.

If you’re involved with managing a Cath Lab have you had your physicians ask to upgrade to a newer digital interventional x-ray system or add high-definition digital large flat screen monitor displays? When planning a remodeling project or lab expansion it is important to have the latest in imaging technology. In order to keep cardiologists happy, or recruit new physicians, hospitals need to be competitive in the local market and provide the newest and highest-quality digital imaging.
But the process to upgrade an x-ray system or add a new lab suite can take time. Starting with budgeting, waiting for funding, approvals, PO’s, and construction schedules it can take anywhere from a few months to a few years to complete.
We’re aware of these challenges and for over 30 years Modular Devices Inc. has offered solutions to lab upgrade and expansions with our interim Mobile Cath Lab and Modular Cath Labs. Our interim Cath and Vascular Lab systems can be quickly and easily brought in and parked at a hospital to provide support on either a short (month-to-month) or long-term basis. Our labs are equipped with the latest digital flat panel detector cardiac/interventional imaging systems, offering an effective way to provide your physicians with newer x-ray imaging technology in the interim while plans are being made to upgrade the in-house lab to new equipment.
In order to properly maintain our fleet of 26 interim labs we’re continually updating the x-ray systems and making other improvements to keep them up to date with the latest technology.
Always listening to our customer’s feedback and reviews we’re very excited to announce the most recent update to our interim lab fleet – large flat screen monitor displays. These high-definition large flat screen monitors measure between 50″-58″ and replace the typical display setup mobile Cath Labs which includes a ceiling-mounted boom with 3 LCD displays (live, reference and hemodynamic monitoring).
In the past we could add additional monitors to the boom for clients who utilize an IVUS system or for 3D EP imaging, for example, but with the large flat screen monitor displays the inputs can be be displayed and rearranged on different sections of the large flat screen display.
This new product roll-out is the perfect solution for long or indefinite term Modular Cath Lab projects where physicians require a large screen monitor in an interim Cath Lab now while they wait for the new lab construction project to be completed down the road.
If you’re interested in learning more about our Mobile and Modular Cath, Vascular Lab solutions can help with a lab renovation or expansion – give us a call at 800-456-3369 or click here to Contact Us.

After connecting the IntelliVue X3 to its docking station at the tableside of the Azurion system, clinical staff can monitor all of the patient’s vital signs including pulse oximetry end-tidal CO2, perform hemodynamic analyses and 12-lead ECG acquisitions, and relay results and waveforms from the lab’s control room to the Azurion tableside display. From the tableside the interventionalists can assess the data using the Azurion tableside Touch Screen Module, allowing them to remain focused on their patients. The system brings the latest physiological techniques to the interventional lab, including iFR (instant wave-Free Ratio) measurements, a hyperemia-free technique unique to Philips that provides valuable functional information regarding the severity of lesions in the coronary arteries.
Philips Interventional Hemodynamic System with Patient Monitor IntelliVue X3 integrates with Azurion, the company’s next-generation image-guided therapy system that allows clinicians to easily and confidently perform procedures with a unique user experience, helping to optimize lab performance and provide superior care. At ACC.21 Philips will showcase its solutions for the diagnosis and treatment of Structural Heart Disease, which aim to remove the barriers associated with complex procedures by helping to deliver clinical confidence where it is needed most – at the point of treatment. Philips’ cardiac care solutions help strengthen clinical confidence, build efficiency throughout the care pathway, and enhance care experiences. For more information visit www.philips.com/acc.
[1] Philips Interventional Hemodynamic System with Patient Monitor IntelliVue X3 is available in the majority of markets worldwide. Philips’ continuous patient monitoring solution is available for sale in markets across Europe, Middle East and APAC, with further expansion planned later this year. It is not available for sale in the U.S.

Minimally invasive, transcatheter therapeutic interventions for structural heart disease have evolved over the past several decades as appealing alternatives to open-chest surgery. Smaller incisions, shorter hospital stays and quicker recovery are outcomes that are ubiquitous to all approved transcatheter procedures, in comparison to traditional surgery. X-ray fluoroscopy (XRF) is the most commonly used imaging modality to guide transcatheter procedures. XRF offers certain advantages. Interventionalists have close familiarity with XRF systems. These systems are also widely available in centers with cardiac catheterization laboratories. XRF can visualize high X-ray attenuating devices such as radio-opaque catheters and metallic stents. However, XRF has certain disadvantages. For example, soft tissues such as myocardium, and valves are visualized poorly. Chambers and vessels are only transiently visible when filled with boluses of iodinated contrast, which can be nephrotoxic in susceptible individuals. Conventional X-ray also images using the principle of “projection” imaging, making it difficult to judge three dimensional (3D) perspective. Finally, over-reliance on XRF as the sole imaging modality exposes the patient and in-room personnel to the harmful effects of ionizing radiation. Wholly magnetic resonance imaging (MRI) (1-4) and ultrasound guided (US) (5,6) cardiovascular interventions have been tested in animal models and clinical studies as ionizing radiation-free alternatives to XRF. However, wide adoption of these methods has been prevented in large part by the lack of visually conspicuous devices that still maintain high mechanical performance.
XRF’s limitations have prompted industry and investigators to improve upon the cardiac cath-lab imaging ecosystem using existing commercial modalities and hardware. The conventional cath-lab commonly offers a pre-acquired MRI or computed tomography (CT) road map, real-time US, electromagnetic (EM) navigation and real-time XRF, all separately displayed on in-room monitors. These separated displays require the operator to cognitively integrate information from these images or imaging streams while they steer devices. A more sensible alternative is to co-register pre-acquired MRI, CT, 3D ultrasound, EM with XRF to provide the interventionalist with well defined, 3D anatomic perspectives so that they can steer devices toward tissues they wish to treat and away from tissues they wish to avoid (Figure 1). Other goals would include reducing the need for ionizing radiation and nephrotoxic contrast and to improve efficiency by reducing the procedure time. Finally, enhanced imaging may even permit novel catheter-based treatments for certain structural heart disorders for which there are no surgical or medical alternatives.
Goreczny et al. (7) report their single center initial experience using VesselNavigator (Phillips Healthcare, Amsterdam, The Netherlands) to co-register and overlay pre-acquired CT/MRI roadmaps onto live XRF using internal anatomic markers. Other commercially available products also perform 3D to 2D XRF fusion such as Siemens Healthcare (Syngo Fusion), General Electric (Innova Vision), and Toshiba (Smart Fusion). In the electrophysiology lab, CARTO sound and CARTO merge utilize EM-3D fusion to guide many interventions. Goreczny et al. performed 2D-3D co-registration for a heterogeneous mixture of pediatric interventions. Image based co-registration was performed using bony structures, calcifications, indwelling devices, or small volume contrast injections. When these experienced interventionalists judged that the co-registration was failing, re-registration was performed during the procedure. The registration was considered subjectively “accurate” in 89% of patients and required intraprocedural adjustment in 22% of patients. There was one patient where re-registration failed due to significant distortion of a vessel due to a large sheath. This paper makes an important contribution to a field that has extensive technical development literature, but is sorely lacking in real-world clinical experience.
Several investigators have made critical advances in improving the cardiac cath-lab ecosystem. Co-registration and display of real-time US, EM, XRF plus static MRI, CT, 3D US road maps (and combinations thereof) have been described (Table 1). Methods for integration of respiratory and cardiac motion correction for MRI roadmaps have been studied in animal models (22). In addition, novel low radiation dose XRF methods for real-time 3D device tracking (23) and real-time 3D ultrasound to provide both anatomic and physiologic information (5) during interventional procedures are future directions of interest. We are not limited to fusion of only two modalities. There are examples of successful fusion of MRI, 3D US, and XRF for guidance of transendocardial injections in swine models (16). We hope one day to have a better interventional imaging eco-system where interventionalists are presented with sensible displays that reliably show devices and their 3D relationship to anatomic structures, where radiation and contrast dose is kept to a minimum and where physiologic consequences of the intervention is rapidly apparent.
Imaging modalityPediatricAdultCT-XRFAortic coarctation, pulmonary artery stenting (9); transcatheter pulmonary valve insertion, venous-venous collateral closure (7)Aortic aneurysm repair (10); transcatheter aortic valve replacement, paravalvular leak closure; pulmonary vein stenting (11)
3DUS-XRFASD closure, Fontan fenestration closure, and transcatheter tricuspid valve replacement (14)Mitral valve repair, left atrial appendage, ASD and paravalvular leak closure (15)

A new Cardiac Catheterization Laboratory is currently under construction and scheduled to open later this summer at the James Family Heart Center at Yavapai Regional Medical Center (YRMC) West. The new Cath Lab includes technology so advanced that it is currently available in only a few hospitals nationwide. This technology will also make YRMC’s new Cath Lab the first of its kind in Arizona.
“The Cath Lab technology is called both world-class technology and world-first technology,” said Lauren Weedon, RN, MSN, Director of Cardiovascular Services at YRMC. “The Cath Lab will be an excellent addition to the Heart Center and for the people we care for throughout our region.”
When it opens, the Heart Center Cath Lab will join two other outstanding Cath Labs at YRMC West. The new Cath Lab is a planned addition to serve patients of YRMC’s Heart Center, including its growing Structural Heart Program.
YRMC’s Cath Labs are equipped with exceptional diagnostic imaging equipment. Interventional cardiologists – specialists who perform non-surgical heart procedures – use that technology to visualize the heart’s arteries, vessels and chambers in order to pinpoint disorders. These physicians then treat their patients’ conditions using imaging equipment to guide and place heart stents, for example.
The Azurion Angiography Operating System – Patients who have undergone past Cath Lab procedures will recognize the angiography operating system as the table they lie on while a C-shaped arm glides around them taking x-ray images. The Heart Center’s Azurion operating system will not only take x-ray images but it also will gather ultrasound images. All of these images will be combined into a single, three-dimensional view of patients’ hearts. Approximately 100 of these Philips operating systems are currently available in the United States.
The EchoNavigator – This technology introduces “road mapping,” which combines the Azurion’s three-dimensional images into a clear and detailed “map” of a patient’s heart. For the first time, physicians will see three-dimensional images of the heart: vessels, valves, leaflets and more in real-time. At the same time, the technology gives interventional cardiologists a sharp view of the catheter or heart implant they are guiding during an angiography procedure.

Pikeville Medical Center’s (PMC) state-of-the-art cardiac catheterization (Cath) labs feature technology and imaging systems that enable physicians to provide cutting-edge care. The equipment offers PMC’s physicians better images of the heart and more sophisticated equipment, allowing them to provide better care.
The PMC Heart and Vascular Institute specialists perform a broad range of minimally invasive procedures, from the most basic to the most advanced heart procedure performed in a cath lab. The technology allows patients to undergo procedures at Pikeville Medical Center that were once performed only in larger cities.
The ability to view multiple images during a procedure can provide quicker and easier results for physicians when caring for a patient. The cath labs at PMC are designed to function as a surgery area to begin the next level of care when necessary.
As an added feature for the patients, each cath lab has a stereo system that plays soothing music to help patients remain calm and relaxed before their procedure. The labs also feature special lighting and monitors that display calming images.
For diagnosis and treatment of coronary artery disease, you demand crystal clear images of the moving heart and of challenging cardiac anatomies in any angulation. To spice up the challenge, dose has to be kept to a minimum even during complex procedures. Our Artis zee systems deliver images in excellent quality and at low dose, displayed the way you like them best with CLEARchoice. A wide variety of software tools supports the toughest percutaneous coronary interventions. Find out how these and other smart solutions from Siemens can support you in your routine and advanced procedures for coronary artery diseases.
ACOM.PC software turns every standard PC into a professional cardiac review workstation. Image processing and diagnostic tools are tailored to the needs of cardiologists, internal medicine specialists, and cardiac surgeons. Connecting to the Artis system, PACS or standard network storage, ACOM.PC can be completely integrated into your department’s IT landscape and also be used as nearline storage offering high-speed access to image data. ACOM.PC can be assigned to a separate display in the examination room for the parallel processing-like review of previous studies during ongoing examinations.
Treatment options for structural heart disease (SHD) are flourishing at a fast pace with the development of new devices, hardware, and software. These technological innovations can replace surgical procedures with percutaneous interventions, often allowing treatment of previously untreatable patients. This leads to new challenges for physicians and their team – as well as for imaging in terms of workflow or multi-modality integration. Siemens’ syngoDynaCT Cardiac has revolutionized cardiac imaging, bringing intra-procedural 3D visualizations of the cardiac chambers and vessels of the beating heart into the cath lab. Based on this technology, we also offer software tools that allow fusion of other 3D imaging modalities like CT or MR for transfer of pre-procedural images used for intervention planning into your ongoing procedure. In addition, you can overlay points of interest or whole 3D structures and acquire peri-procedural 3D images for improved guidance during demanding SHD or vascular procedures. Dedicated workflow support tools facilitate procedures like transcatheter aortic valve replacement (TAVR). Find out how our solutions can support you in the dynamic and fast changing environment of SHD treatment.
Create CT-like images of the heart in your cath lab using rotational angiography – with syngo DynaCT Cardiac. The high-quality 3D images support you in analyzing the cardiac anatomy to plan and guide complex SHD procedures. Fuse 3D volumes acquired with other modalities or mark regions of interest in pre- and intra-procedural 3D images, which can be overlaid onto live 2D images. Here as well, linking the C-arm to a 3D image helps you define the optimal projection angle – without additional contrast media or fluoroscopy.
syngoiGuide Toolbox allows you to overlay points of interest from 3D volumes onto 2D live images right on the Artis display. Using the linked cursor feature, you can quickly and easily import the points of interest into the 2D live images ‒ exactly matching the findings in the cross-sectional images of a syngoDynaCT Cardiac acquisition, for example. It takes just a single click to create anatomical outlines of segmented 3D volumes, which can be especially helpful for mitral valve repair or for vascular procedures like aortic aneurysm stenting. The information that is overlaid using syngoiGuide Toolbox is automatically updated should you change the C-arm angulation, the zoom factor or move the table.
Covering everything from imaging and recording to 3D guidance and co-registration with the latest mapping and navigation systems. Smart solutions designed to set new standards of care, safety, and efficiency for your EP lab.
With the help of rotational angiography, syngo DynaCT Cardiac creates CT-like 3D images of the beating heart directly in your cath lab. There is no need for pre-procedure CT, and you get high-quality 3D volumes during the case. ECG-gated acquisition enables visualization of the coronary sinus and the ventricles for procedure planning. Special low-dose algorithms can be used to fuse 3D angio images with CT and MR.
With its convenient one-click segmentation, syngo InSpace EP allows you to quickly and effectively segment the cardiac chambers, thus reducing time-consuming manual interactions. Excellent AFib ablation planning by visualizing the individual LA morphology, improved orientation and catheter guidance during mapping and ablation and esophagus visualization for reduced risk in AFib procedures are three benefits. It allows you to view inner surfaces of segmented chamber with a clipping function and an easy point tagging function to plan the ablation path and for documentation purposes.
Enhance catheter guidance during ablation with syngo iPilot. Application provides an overlay of 3D segmentation results (from syngo DynaCT, CT or MR) onto live fluoroscopy. It allows overlaying pre- and intra-procedurally acquired 3D volumes onto live fluoroscopy or acquisition.
The dual-volume visualization for enhanced decision-making during intervention enables the differentiation between two high-contrast 3D objects that have virtually the same contrast density or allows the display of syngoDynaCT and 3D Angio in one view.
Enables previous CT, MR or PET CT images to be fused with high-contrast angio 3D or syngoDynaCT datasets. syngoInSpace 3D/3D Fusion not only displays relevant diagnostic data from other modalities in the angio suite but serves as foundation for exact overlay of 3D volumes and planning data onto live fluoroscopy during treatment (using syngoiPilot®).
Effective device guidance during interventional procedures, providing a simultaneous display of the live fluoro, roadmap or acquisition image and a matching 3D volume or planning data to facilitate guidance during complex interventions. The system updates dynamically to movements of the C-arm, table, zoom, and source-to-image distance.
A 3D functional imaging application that provides physiological information directly in the interventional lab. The software indicates the distribution and amount of blood in lesions and surrounding tissue by means of color-coded cross-sectional blood volume maps.
EVAR-3D Guidance overlays 3D information on top of live fluoroscopy and stands for optimized C-arm angulations, precise 3D overlay, and guidewire and catheter navigation.




 Ms.Josey
Ms.Josey 
 Ms.Josey
Ms.Josey